Irritable Bowel Syndrome (IBS) is a common disorder of the gut-brain axis estimated to impact one in five Australians at some point in their life and is generally more common in women than it is in men1.
IBS is a complex condition that often requires a combination of treatment and management strategies to effectively manage a patient’s symptoms. No two cases of IBS will ever present identically, and it is likely that the management strategies involved will differ between patients.
What is IBS and how is it diagnosed?
The diagnosis of IBS is often based on symptoms after the exclusion of other possible gastrointestinal diseases. IBS can be categorised into four major subtypes depending on the predominant stool pattern:
It should be noted that these subtypes are not considered distinct, and instead represent the spectrum of clinical presentations that vary in quantity, intensity, and severity of symptoms between patients.
What are the main causes of IBS?
Although the precise cause of IBS is still unknown, it is thought that IBS involves a complex interaction of many factors, including microbial dysbiosis, visceral hypersensitivity, altered mucosal immune function and changes to the brain’s regulation of gut function2.
Around 9% of IBS is thought to be post-infective IBS which was triggered by a gut infection3. Age, genetics, diet, and stress are also known to play a role in the onset of symptoms associated with IBS2.
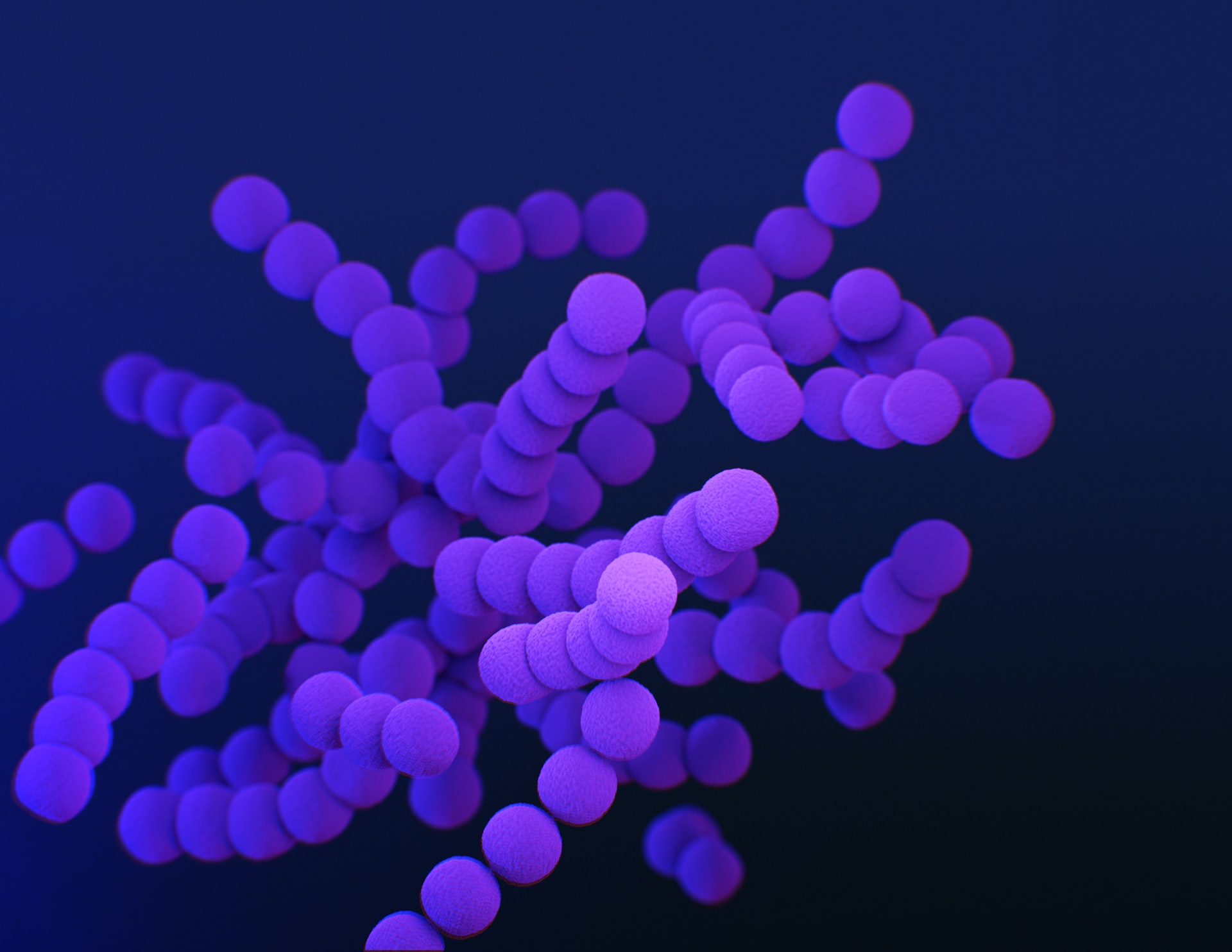
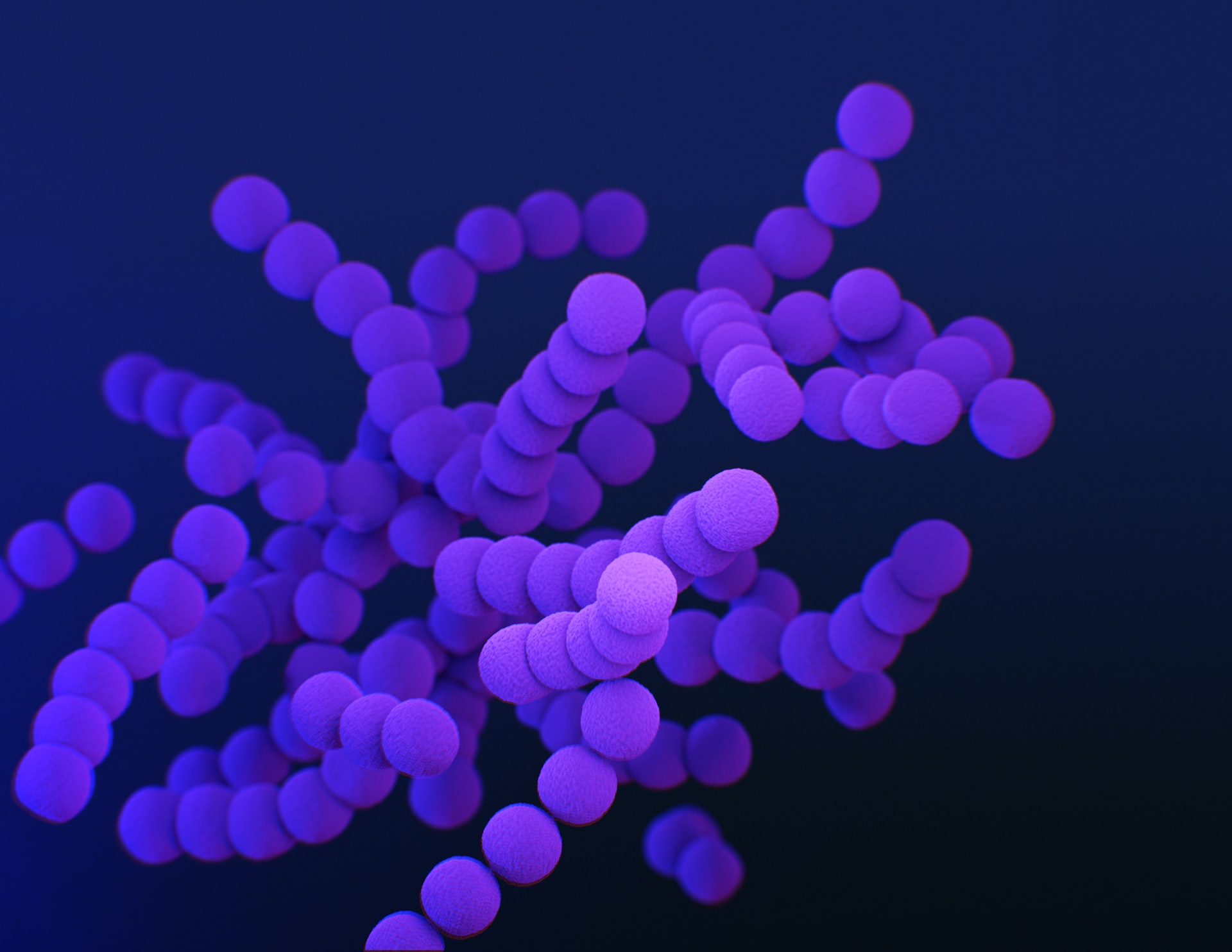
What are the known associations between the gut microbiome and IBS?
The gut microbiome is associated with many areas of health, including gastrointestinal health, and associated medical conditions. A growing body of evidence is looking to understand how the gut microbiome differs in people who have IBS compared with those who do not.
Emerging research is revealing recurring patterns are evident in the microbiomes of individuals who have IBS4-6. These include:
The value of gut microbiome analysis for IBS sufferers.
As we now know, significant microbial dysbiosis is seen in IBS sufferers. However, the characteristics of the dysbiosis will differ patient to patient. Using metagenomic analysis we can understand the dysbiosis allowing us to tailor the intervention for the promotion of microbial balance.
Book a Microbiome appointment with Dr McAdam or Dr Cheong to discuss testing. But first see your Gp to have your bowel symptoms fully investigated for other causes first.
Extra Medicare benefits are now available to eligible patients who have registered with the Australian Government’s MyMedicare eg longer telehealth appts, care plans and mental health plans. WE offer 7 day access (Telehealth on Sundays) and you can still see your local practice if you need to when registered with us. To register or learn more about how MyMedicare can benefit you, click here or ask on arrival
There are multiple ways you can register with your chosen practice in MyMedicare:
MyMedicare registration will not prevent you from accessing care from other practices and healthcare providers. MyMedicare does not tie you to a particular healthcare provider. You can change your preferred GP within your registered practice at any time.